Surgeries :
Surgery is an ancient medical specialty that uses operative manual and instrumental techniques on a patient to investigate and/or treat a pathological condition such as disease or injury, to help improve bodily function or appearance or to repair unwanted ruptured areas. The scope of surgery is determined by the type, size, and location of cancer.
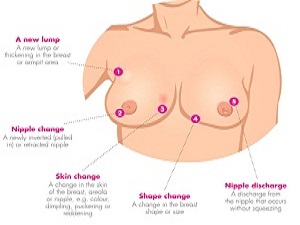
1. Brest Cancer :
Surgery involves the physical removal of the tumor, typically along with some of the surrounding tissue. One or more lymph nodes may be biopsied during the surgery; increasingly the lymph node sampling is performed by a sentinel lymph node biopsy.
Standard surgeries include :
- Mastectomy: Removal of the whole breast.
- Quadrantectomy: Removal of one-quarter of the breast.
-
Lumpectomy: Removal
of a small part of the breast.
Dr. Vinod Gore is one of the experienced Breast Surgeon in Pune. He has been trained at Tata Memorial Cancer Centre Mumbai. Presently he is working as a consultant Cancer Surgeon at all prime institutes at Pune like Sahyadri Hospital, RUBY Hall Clinic, Noble Hospital, and Inamdar Hospital Pune.